“Critical Thinking for 21st-CenturyMedicine—Moving Beyond Illness Scripts”
Clinical Reasoning for 21st-Century Medicine:
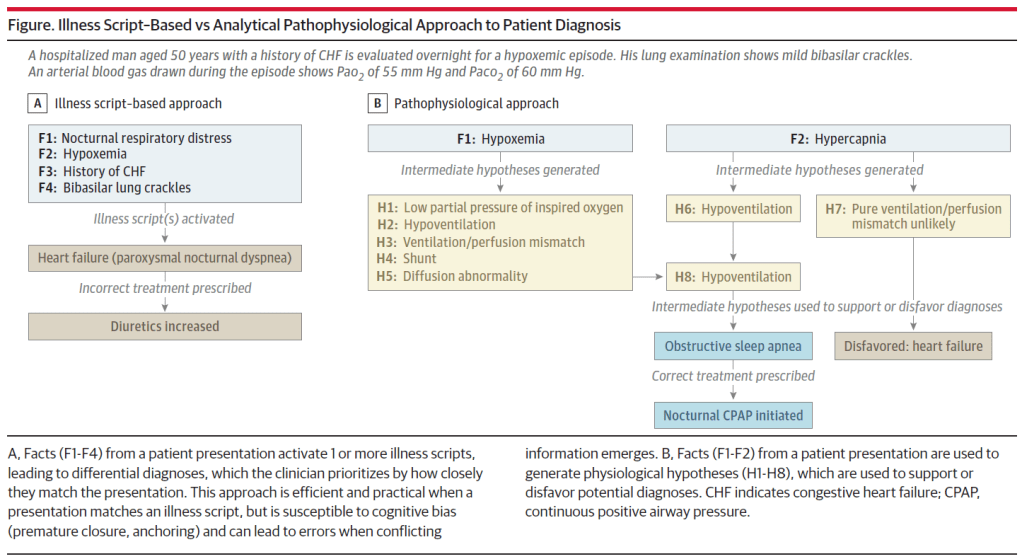
Optimal clinical reasoning will involve an appropriate balance between
illness scripts and pathophysiological reasoning.
In our view, medical education has historically overemphasized the former—to which learners are predisposed even without explicit teaching— and underemphasized the latter.
The risks of this historical approach will become even more salient as generative AI, especially in the form of large language models, assumes a greater role in clinical evaluation and diagnosis.
AI excels at pattern recognition. As large language models and their training data improve, AI will likely outperform human diagnosticians, especially in routine cases that cohere with prototypical illness scripts. Human physicians should develop complementary skills that machines can less easily replicate, such as flexible reasoning, creative problem-solving, and the ability to navigate uncertainty in cases involving new knowledge and/or unfamiliar presentations.
To the extent that medicine represents a “wicked” environment —marked by complexity, incomplete rules, and delayed or inaccurate feedback— it is less amenable to AI, suggesting that efforts to teach clinical reasoning should prioritize flexibility and nuance over automaticity.
Now more than ever physicians must build their practices on the
foundation of strong critical thinking skills. In the 21st century, this
means medical education must go beyond teaching students what
to think and instead teach students howto think when patterns do
not fit (or how to verify when patterns do seem to fit). By questioning
a primary focus on illness scripts, emphasizing pathophysiological
reasoning, and cultivating adaptive expertise, we can prepare
future physicians—and their patients—for what may lie ahead.